| TOPIC | Delirium Identification and Response Procedure | ||
| AREA | Service Delivery | TYPE | Procedure |
1. Purpose
Mobility is committed to providing safe and effective care. This procedure outlines how a consumer with delirium is identified early to reduce any adverse outcomes relating to the deterioration in a consumer’s mental state by early recognition and effective response.
2. Scope
This procedure applies to all support workers, others who support consumers face to face and Registered Nurses (RN) who manage the consumers care planning.
3. Definitions:
| Delirium | Delirium is a change in mental status that can be triggered by illness, surgery, injuries, or adverse effects of medicines. Some consumers are more likely at risk of delirium than others. Consumers with delirium experience disturbances in consciousness, attention, thinking and perception. These changes develop over a short period of time (usually hours to a few days). Consumers with delirium may be agitated and restless or quiet and withdrawn. As well as being distressing for the person experiencing it, delirium is a serious health condition.[i] |
| Acute Deterioration | Acute deterioration includes physiological changes, as well as acute changes in cognition and mental state. |
| Support Workers | Includes all Personal Care Workers (PCW), RN and EN. |
4. Roles and responsibilities
Support Workers – Personal Care Workers (PCW), RN and EN
- Use the consumers care plan to guide monitoring of consumers who are at risk of acute deterioration in their mental state, incorporating knowledge from the consumer, and their carer and families about individual early warning signs.
- Monitor the consumer after discharge from hospital as the risk for delirium is increased after surgery.
- Support workers are to be alert to signs of deterioration in a person’s mental state, including for consumers who have not been previously identified as being at high risk.
- If the consumer has a care plan from the discharging hospital – support workers are to follow the care plan and report any changes to the consumer’s condition to mobility.
- Implement and follow the GP care plan once there is a clinical diagnosis.
- Advise mobility immediately if there are concerns regarding delirium and call 000 and keep the consumer safe.
RN Care Planning
- Discuss with the consumer, and/or authorised representative of any early warning signs if indicated.
- Make recommendation for formal clinical diagnosis by the consumers GP to the consumer or authorised representative.
- Review and update the care plan.
- Advise the consumer, care manager and clinical & risk specialist (CRS).
5. Procedure
5.1 How to identify a consumer with delirium
Consumers with delirium may:
- Appear confused and forgetful
- Be unable to pay attention
- Be different from their normal selves
- Be very agitated, quiet, and withdrawn, sleepy, or a combination of these
- Have rapid and unpredictable mood changes
- Be unsure of the time of day or where they are
- Have changes to their sleeping habits, such as staying awake at night and being drowsy during the daytime
- Feel fearful, distressed, upset, irritable, angry, or sad
- Hallucinate and see frightening things that are not there but seem very real to them
- Lose control of their bladder or bowels
- Have delusions or become paranoid, and strongly believe things that are not true – for example, they may believe that someone is trying to physically harm them or has poisoned their food.[ii]
These symptoms fluctuate during the day and may worsen in the evening or night.
Family members, carers or support workers can support the consumers by:
- Reassuring the consumer
- Reminding the consumers about eating and drinking
- Having familiar objects near the consumer
5.2 Response Procedure
Risk of Delirium – diagnosis NOT confirmed
- If you suspect the consumer is displaying signs of delirium, a cognitive and physical function assessment needs to be completed. Refer the consumer to their GP for a formal diagnosis or call 000 if you have immediate concerns for the consumers safety and contact mobility.
- Consumers need to be monitored in particular after a hospital visit as there is an increased risk of delirium after surgery in the elderly.
Procedure when a diagnosis is confirmed
Follow the plan from the GP and monitor for changes in behaviour, cognition, and physical condition. The plan will have ways to prevent falls and having an injury from a fall, such as wearing safe footwear or hip protectors, and care to prevent pressure injuries.
The plan may also have:
- a nutrition plan to prevent malnutrition and dehydration
- a summary of changes in medicines; and
- any other ongoing treatment.
The consumer is to be encouraged to keep mobile and family or carers are to be encouraged to be involved in the consumer’s care.
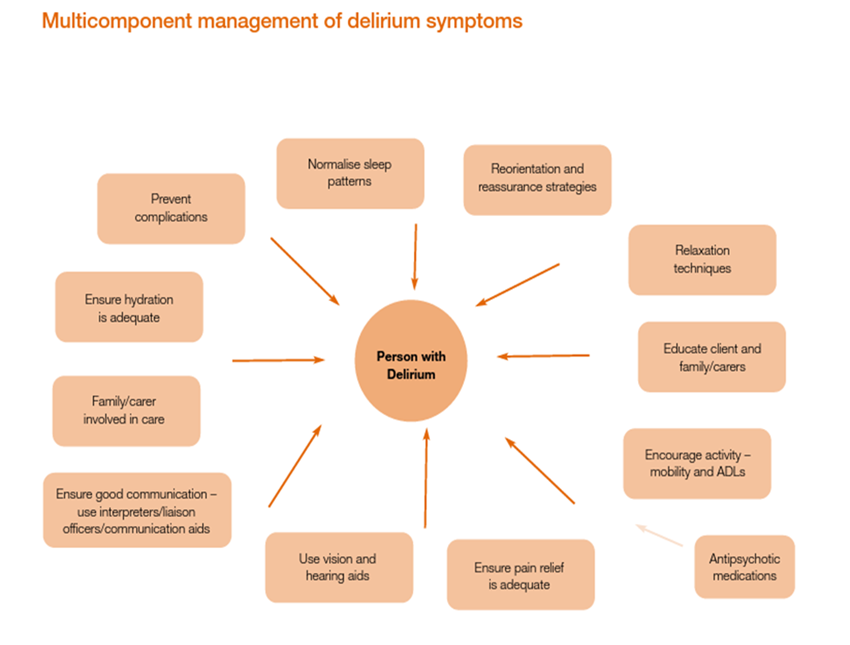
The below diagram shows the management response for a consumer diagnosed with delirium.
[iii]Clinical Epidemiology and Health Services Evaluation Unit 2006, Clinical practice Guidelines for the Management of Delirium in Older People, Victoria Government Department of Human Services, Melbourne, Victoria.
Promote good sleep habits
To promote good sleep habits:
- Provide a calm, quiet environment
- Keep inside lighting appropriate for the time of day
- Plan for uninterrupted periods of sleep at night
- Help the consumer keep a regular daytime schedule
- Encourage self-care and activity during the day
Promote calmness and orientation
- To help the consumer remain calm and well-oriented:
- Provide a clock and calendar and refer to them regularly throughout the day
- Communicate simply about any change in activity, such as time for lunch or time for bed
- Keep familiar and favourite objects and pictures around, but avoid a cluttered environment
- Approach the consumer calmly
- Identify yourself or other consumers regularly
- Avoid arguments
- Use comfort measures, such as reassuring touch, when appropriate
- Minimise noise levels and other distractions
- Provide and maintain eyeglasses and hearing aids [iv]
Prevent complicating problems
Help prevent medical problems by:
- Giving the consumer the proper medication on a regular schedule
- Providing plenty of fluids and a healthy diet
- Encouraging regular physical activity
- Getting prompt treatment for potential problems, such as infections or metabolic imbalances
6. Related Documents
6.1 External Documents
- Aged Care Quality Standards
- Aged Care Quality and Safety Commission Act 2018
- Aged Care Quality and Safety Commission: Clinical governance in aged care
- https://www.safetyandquality.gov.au/publications-and-resources/resource-library/clinician-fact-sheet-delirium-clinical-care-standard
- https://www.mayoclinic.org/about-mayo-clinic
- Clinical Epidemiology and Health Services Evaluation Unit 2006, Clinical practice Guidelines for the Management of Delirium in Older People, Victoria Government Department of Human Services, Melbourne, Victoria.
- Aged Care Act 1997
- User Rights Principles 2014
- Quality of Care Principles 2014
- Aged Care Quality and Safety Commission Rules 2018.
- Charter of Aged Care Rights
- Privacy Act 1988
- Australian Privacy Principles 2014
- Australian Commission on Safety and Quality in Health Care
6.2 Internal Documents
- Clinical Governance Framework
- Model of Care
- Medication Management Procedure
- Medication Prompting Procedure
- Swallowing and Choking Procedure
- Personal Care Worker Procedure
7. Document History
Reviewed by: Clinical and Risk Specialist
Authorised by: CEO
Date Adopted: August 2022
Next Review Due: August 2025
Version Control
| Version | Date | Change |
| 1 | 16/5/22 | New |
[i] Dementia Australia (2015) Delirium and Dementia Fact Sheet Question and Answer https://www.dementia.org.au/files/helpsheets/Helpsheet-DementiaQandA21_Delirium_english.pdf
[ii] Dementia Australia (2015) Delirium and Dementia Fact Sheet Question and Answer https://www.dementia.org.au/files/helpsheets/Helpsheet-DementiaQandA21_Delirium_english.pdf
[iii] , [iv] Dementia Australia (2015) Delirium and Dementia Fact Sheet Question and Answer https://www.dementia.org.au/files/helpsheets/Helpsheet-DementiaQandA21_Delirium_english.pdf